Contribution of Dr Saurabh Kole on disaster management
through diffrent organisation since 2001

Disasters, their management and medical professionals have been closely associated for a very long time. Many path-breaking medical procedures, discoveries and protocols were born on the battlefields during wars, which are man-made disasters of the greatest level. Involvement of medical professionals in disaster management has benefited not only the victims but also enriched the science and its practitioners with valuable experience. Even in today’s world of super-specializations and niche practice, medical professionals must be in the forefront when disaster strikes. But they should be adequately prepared for it.
World Health Day is celebrated each April 7 to mark the founding of the World Health Organization. In 2009, World Health Day’s theme is when Disasters Strike: Safe Hospitals Save Lives. It focuses on three important messages: All health facilities must be able to withstand the physical impact of disasters; critical health services must continue to function in all emergency situations; and the health workforce must be trained and ready (prepared) to deal with the particular challenges these situations impose.
Disaster -
“A serious disruption of the functioning of the community or a society causing widespread human, material, economic or environmental losses which exceed the ability of the affected community or society to cope using its own resources” United Nations
| Natural | Earthquake, cyclone, floods, volcanic eruptions, wild fire, draught, tornado |
|---|---|
| Man-made | War, biological warfare, chemical warfare, fire, nuclear hazards, gas and chemical poisoning, |
The boundary between natural and man-made disasters is often blurred. Hazards can range from an earthquake, which is of natural origin; to a landslide, which can be caused by a combination of deforestation, heavy rains and light earth tremors; to a chemical spill, which is man-made. Climate change is increasingly blurring the distinction between man-made and natural hazards. Although climatic hazard, such as droughts and floods, would occur regardless, global warming may increasingly modify these types of hazards.
Hazard Identification and Vulnerability Assessment (HIVA)
The first step toward a mitigation program is the identification of the hazards a community may face. Largely, local hazards can be categorized as either natural or technological/manmade events. While the local climate changes rather slowly, our manmade environment can change rapidly, especially in terms of the local economic base.Hazards are assessed comparing the experienced frequency of the event versus the potential impact that may result.
| High Probability Low Impact | High Probability Moderate impact | High Probability High Impact |
|---|---|---|
| Moderate Probability Low impact | Moderate Probability Moderate Impact | Moderate Probability High Impact |
| Low Probability Low Impact | Low Probability Moderate Impact | Low Probability High Impact |
Probability vs. Impact
Planning begins with events that are expected to occur often and have potentially high impacts on life and property followed by those with more moderate probabilities or moderate impacts. Jurisdictional strategies are dependant on the philosophy and experiences of local officials. Largely, the priorities addressed in HIVA years one through five are a reflection of this assessment and local philosophical priorities. For the purpose of this document, the criteria for high, moderate, and low probability are:
High Probability: once a year
Moderate Probability: once every two to ten years
Low Probability: once every ten to fifty years
A Medical disaster occurs when the destructive effects of natural or man-made forces overwhelm the ability of a given area or community to meet the demand for health care
Challenges posed by disaster
Disaster related loss is on the rise with grave consequences for the survival, dignity and livelihood of individuals, particularly the poor and hard-won development gains. Disasters in one region can have an impact on another part, and vice versa. This, compounded by increasing vulnerabilities related to changing demographic, technological and socio-economic scenarios, environmental degradation, climate variability, climate change, geological hazards, competition for scarce resources, and the impact of epidemics such as HIV/AIDS, points to a future where disasters could increasingly threaten the world’s economy, and its population and the sustainable development of developing countries. In the past two decades, on average more than 200 million people have been affected every year by disasters.
Disaster preparedness:
Country/ state specific details, like disaster proneness, previous history of disasters, geography and topography, distances between capital city and disaster-prone areas, national and local disaster response and management capacity, security, maps, existence of early warning and other alarm systems, existence of relief agencies and disaster capacity of sister agencies, as well as local customs/ norms and other information about common and possible natural hazards can be obtained to form a plan.. The Humanitarian Early Warning Service website (www.HEWSweb.org) is a global one-stop shop for early warning information. It has dedicated pages for drought, floods, topical storms, locust infestation, El Nino, earthquakes and volcanic activity, including additional references and resources. The site, whose homepage displays a natural hazard map of the world with the various risks facing specific countries and regions, rationalizes and brings together under one platform the vast amount of information now available on the internet from multiple specialized institutions.
Strengthening the health surveillance system:
Reporting and surveillance system must be restored and reinforced from the earliest stages of a disaster. This is a high priority in any emergency because health information systems allow the identification of problems, in particular potential outbreaks of communicable diseases. At a minimum, the reports should cover the main killer diseases (measles, malaria, ARI, mal nutrition, diarrhea) and other epidemic-inducing diseases according to epidemiological context (meningitis, yellow fever) reports should produce reliable information on death rates.
Attitude towards disaster
“What the scientists can not predict is described as wrath of nature… as science advances the mystery behind the wrath shall be unveiled and a more rational understanding of natural disasters shall be possible”, wrote Bertrand Russell in Science and Religion. Preparedness is the key word. In Developed countries there is system of a such preparedness building by providing a system of enhancing knowledge, skill and attitude within the disaster hit communities as well as the responding teams and agencies. But unfortunately this concept is still in a very nascent stage in the mindset of a developing country. As a result the impact of same event is felt with more vigor and intensity in South-East Asia than by any developed country. Experiences tell that Health care receives further setback as most of the health infrastructure also suffers serious damage rendering them non-functional and unable to provide any help to the stricken community. Natural disasters are striking South-East Asia with unfailing regularity killing thousands of people every year and rendering millions homeless and dependent on external assistance for survival. These days’ situations have been complicated further as more and more man-made disasters are striking the humanity in a complex setting of political world. It is in this perspective that disaster preparedness is promoted, practiced and planned at all levels primarily to restrict the damage and loss suffered, prevent/mitigate health fatalities/emergencies that might have struck the receivers of these natural and human induced calamities. We cannot afford to ignore this aspect anymore.
Why Critical Care Society:
In common parlance Critical Care implies addressing sudden acute health crisis by a range of Health Specialists. In Disaster situation and particularly in terms of preparedness, Critical care gives a feeling of emergency response rather than preparedness. But to respond in highly demanding situations, the response team must be clear in mind what their expected roles are and what they need to do given the situation. The element of Preparedness comes into play here. Unless a team of Critical care professionals are prepared how to face the horrible ground realities that may warrant imminent variety of medical and surgical actions with expectations often differing in realities, the outcome of interventions may not yield desired goals. In this perspective Disaster Preparedness is equally important for Critical Care professionals though slightly different from preparedness activities prescribed for professionals from other fields.
As a discipline, critical care personnel are used to rapid response, teamwork, working against odds, working round the clock and doing all these almost by reflex, thereby saving crucial time and preventing delay.
A huge variety of medical problems and complications can be encountered in a disaster-affected area. Not only that, a trivial illness or injury tends to aggravate rapidly in an already stressed person in a disaster-affected area. This is precisely why critical care specialists have such an important role to play. As a Critical care professional I have a variety of experiences of rendering service in disaster situations. The entire health system in Bhuj, Gujarat, collapsed after a massive earthquake. A team of ten Doctors and Paramedics (Ten) from Kolkata visited the ravaged area after about a week of the incident. The experiences varied from multifarious fractures inflicted by the earthquake to delivery of a newborn in makeshift medical camp. A doctor of local hospital was admitted in that camp following an acute myocardial infarction and treated by the Critical care team within limitations of infrastructure and subsequently cured to possible extent. A Disaster management committee was formed by the Critical care society following Gujarat experience. The objective was to provide prompt limited but critical medical support to local institutions in the wake of events with high degree of severity and damage. Following the devastating Tsunami Critical Care Society provided service to the community by its committed presence at Nagapattinum and Kadalur situated in coastal Tamilnadu and worst hit by the event and also in Port Blair Andaman.
A mother running to escape Tsunami waves in Andaman Islands in 2004 December with four children and gradually losing all of them finally received fracture in neck femur with multiple injuries by being smashed against a tree by lashing waves had to be treated by the critical care unit as a traumatized patient. The priority in this case varied from trauma counseling to fixing her broken leg along with prevention of infection and sepsis. Gaining valuable experience in Gujarat, we from Indian Society of Critical Care Medicine thought of spreading our initiatives in other countries as well. In the recent experience of Bangladesh Cyclone (Sid-r) and Myanmar cyclone (Nargis), with the help of Rotary Club Dist. 3290 Critical Care Society worked as support unit in two hospitals, one at Sarankhola of Bangladesh (most affected area) and the other at Dala of Myanmar. A relief team was sent to the affected areas of Bangladesh consisting of Doctors of different disciplines, logisticians, Technicians and Para Medics. The target area was Sarankhola in the District Bagerhat at the bank of Dholeswari. The cyclone massacred not only human lives but also property and the animal husbandry. The worst affected area was the core of Sunderban causing massive loss in ecology and wildlife. The journey itself showed the massive devastation, which were scattered beside the roads leading towards Sarankhola. More than 1000 patients visited the medical Camp most of who were mainly suffering from high fever, gastroenteritis and orthopedic trauma. A medical team was sent to Myanmar on August 2008 when the Government of Myanmar decided to open up the doors to the foreign aid teams to the areas affected by the Cyclone, Nargis. Our team was allotted Dale, a village that was affected by the Cyclone at the bank of Yangon River. The team organized a five full day medical camp in the PHC of Dale. More than 1500 patients visited the camp.

Immediate Aims of Disaster Management
- To Save Lives
- To Reduce Loss
- Emergency Relief
- Provide security and confidence to the affected community
Objectives of Disaster Management
- To minimize human loss- physical, economical & environmental
- To reduce personal suffering
- To achieve rapid and durable recovery
Hospital in Disaster Management
Hospitals are supposed to be the centre of providing care to disaster-affected areas. There have been ideas going around on how best to equip hospitals to respond to a disaster. The WHO has provided the following guidelines;
WHO Benchmarks for Hospital Preparedness and Response
- 1. Legal and institutional framework for EPR/li>
- 2. Disaster preparedness plan and Standard Operating Procedure
- 3. Financial, physical and human resource allocation and accountability
- 4. Rules of engagement for external humanitarian agencies
- 5. Community plan for mitigation, preparedness and
- 6. Community-based response and preparedness capacity
- 7. Local capacity for emergency provision of essential services and supplies (shelters, safe drinking water, food, communication)
- 8. Advocacy and awareness through information, education, communication
- 9. Capacity to identify risks and assess vulnerability at all levels
- 10. Human resource capabilities continuously updated and maintained;
- 11. Health facilities built/modified to withstand the forces of expected events
- 12. Early warning and surveillance systems for identifying health
Quick Response Medical Teams
- • Every hospital must develop QRMTs and train them with state-of-the-art facilities of quick and coordinated response in emergency situations
- • QRMTs must be supported by minimum facilities of emergency
- • QRMTs of different hospitals at city level must be networked to come to each other’s assistance in emergency situations
Specialized facilities for Chemical, Biological, Radiological and Nuclear (CBRN) Disasters:
- • CBRN disaster require specialized facilities for decontamination, Personal Protective Equipments, detection equipments etc
- • These facilities are grossly lacking even in our tertiary care institutions
- • Training programs for doctors, nurses and paramedics on CBRN management are also inadequate
“In disasters, hospitals should not be allowed to become victims too," said PAHO (Pan American Health Organization) Director Dr. Mirta Roses. ". The cost is lower than what one might expect and far less than the price paid when health facilities fail at the time when people need them most."
In Geneva recently, the World Health Organization (WHO) called on its member countries to undertake six core actions to make their health facilities safe during emergencies:
- 1. Assess the safety of hospitals
- 2. Protect and train health workers for emergencies
- 3. Plan for emergency response
- 4. Design and build resilient hospitals
- 5. Adopt national policies and programmes for safe hospitals
- 6. Protect equipment, medicines, and supplies.
PAHO has developed a Hospital Safety Index that is being used by a number of countries in Latin America and the Caribbean to assess the level of safety of their hospitals and health facilities, and to determine what steps are needed to improve their safety. One of the most important lessons from Katrina was that generators and other critical utilities should not be located on the lower floors of health facilities, where they are most vulnerable to floodwaters.
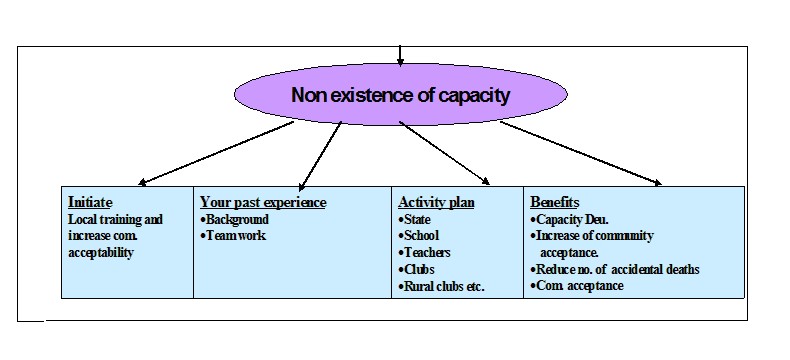
Public-private collaboration in disaster preparedness is also critical, according to Chris Van Gorder, president and CEO of Scripps Health, which operates five acute-care hospital centers in California. "Hospitals need to be part of local preparedness plans. We have to collaborate with local, state, and federal agencies, and for that to happen, we need to plan and practice in advance." Health system strengthening and community capacity building are two parallel exercises and should go hand in hand. The following picture represents capacity building on disaster preparedness at various levels.
Disaster Management framework as recommended by the Government of India:
Agencies involved for Disaster management:
– Department of Science and Technology
– Department of Space
– Ministry of Water Resources
– Department of Ocean Development
Emergency Operation Centers:
- • State-of-the-art Emergency Operation Centers established in Ministry of Home Affairs for data, video and audio up-linking with all State, District and remote areas
- • EOCs being set up in all State, Union Territory and District headquarters
- • India Disaster Resource Network (IDRN) -web-enabled, centralized inventory of resources established - www.idrn.gov.in
- • Over 80,000 records from 565 districts of 35 States/ Union Territories uploaded.
Mass casualty management
- • Our health system is not fully geared to face mass casualty events where a large number of people get affected resulting in high degree of morbidity and mortality
- • Our country is in the process of setting up an effective disease surveillance system backed by early warning, communication, transportation and evacuation of casualties, training and capacity development etc.
Need of the hour:
We suggest that critical care societies from each region have a Rapid Response Team and protocol ready. A Makeshift hospital with equipment and facilities to provide adequate service should be planned and be ready on demand. Proper education for doctors and health-workers to tackle disasters most effectively must be an essential and on-going feature of our society.
Conclusion:
Once you choose hope, anything's possible. It’s this message that rang out, loud and clear, from the rubbles of earthquake to the devastation caused by the Tsunami.
Critical Care Experts, in different parts of the world, have played a crucial part in responding to the health emergencies arising out of disasters. A network among such societies would also help to coordinate the activities and exchange of experts in different fields on the basis of felt needs. The system can be institutionalized and gradually built to rise to the demands created during emergencies by providing proper medical care to the disaster victims. We need to accept that Critical care is now on its move out of the secured zone of intensive care to broader horizons where scores of people are in need of medical attention following a disaster which could save their lives and limbs. Let us organize ourselves with determination to stand by the people who are in distress and look up to us with utmost expectations.In the same breath I would like to add that Japan has shown the world over the years how inculcating the culture of Disaster Preparedness has helped the nation cope with the extremities of terrible natural Disasters, as also the nuances of Critical Care as a part of Disaster Preparedness. This exposure will be extremely helpful for me to learn about your practices and broaden my humble contribution to the stricken community in Critical Care.
References:
- 1. Fundamental Disaster Management – Society of Critical Care Medicine
- 2. Paradigm Shift in Disaster Management by Mr. P D Dhar Chakraborty - Director National Institute of Disaster Management, New Delhi
- 3. Health Facilities In Emergencies : World Health Organisation -
- 4. Disaster Preparedness & Experience of Disaster Management; Dr S. Kole; National Conference Brochure ISCCM 2009
Acknowledgement:
- Mr. Pinaki Halder
- Dr S. K Biswas
- Dr Rajarshi Dutta
- Mr. Chandan Kumar De
- Mr. Chandra Sekhar Biswas
- Ms. Dola Dutta Roy
Team of Disaster Management Committee
| Dr. Sumit Poddar, | Dr. Bimal Roy, | Dr. Jyotsna Paranjape, |
|---|---|---|
| Dr. M. M. Roy, | Dr. Asitendu Dutta, | Dr. K. Saha, |
| Dr. Amit Roy, | Dr. Debasish Sarbadhikari, | Dr. Saurabh Kole |
| Mr. Goutam Roy, | Mr. Joy Roy Chowdhury, | Mrs. Dipali Poddar, |
| M. Kasim, | Ms. Anndhi Sha, | Mr. Kaustuv Chatterjee,Dr.Gautam Saha and Many Others |

 Home
Home About AHCF
About AHCF Events
Events Contact
Contact